I recently got shortlisted to present a Case at the Health Education England Midlands and East DCT Showcase. My case included many disciplines including restorative, endodontics, oral surgery and prosthodontics. I hope you find it an interesting read and please feel free to make some comments!
Introduction:
A 21-year-old female (Miss X) presented with pain from LR7 and was concerned regarding the acquired edentulous space around ULQ. She was assessed and treated in general dental practice.
SH: Miss X is a Law student, studying for long hours with a potential cariogenic diet. She does not smoke and occasionally consumes alcohol.
MH: Fit and well, no allergies or medications reported.
DH: Heavily restored adult dentition, moderate OH. Diet history revealed a cariogenic diet.
Presenting Complaint:
“My lower right bottom tooth is crumbling away and so is the top left one!
I hate that I have a gap when I smile…. I’ve lost my confidence!”
Diagnoses:
1. Generalised plaque induced gingivitis
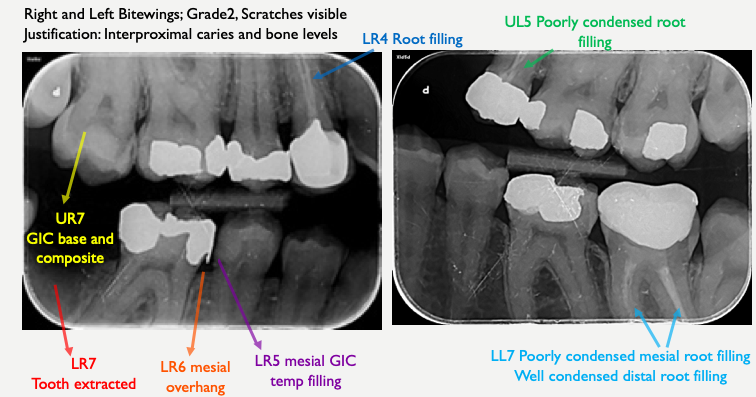
2. Chronic periapical periodontitis LR7
3. Secondary Caries LR5
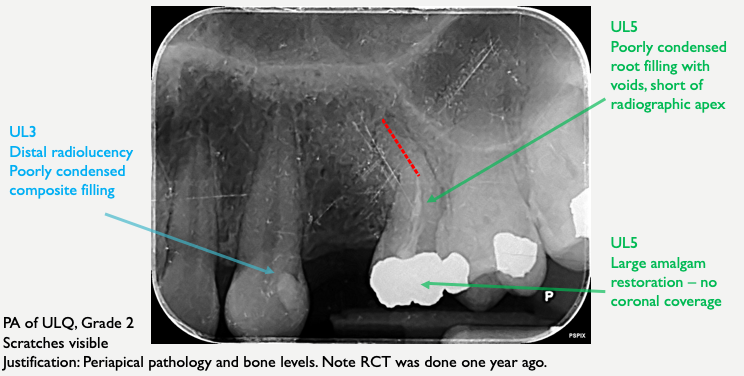
4. Suboptimal RCT UL5- poorly condensed and short of the apex
5. Acquired edentulous space UL4
Pre Operative Photographs:

Pre op Radiographs:
Aims and Objectives of Treatment:

The Treatment Plan:

Plan of Treatment:

Operative clinical photographs:

Post Operative Photographs:


Occlusion:


Keep it clean!

Post Obturation- RE-RCT of UL5

At first glance, it may appear that I have extruded. However, I carried out a 3 month review and in the abcense of signs and symptoms such as sinus involvement, pain or swelling, I am confident the GP is within the radiographic apex.
The image below shows where I believe the apex ends in green. The red line indicates a different outline of the root morphology indicating that I have extruded.
The only way to be certain my root filling is within the apex is to carry out a CBCT scan which we do not routinely perform in endodontics.

3 Month Review:

Evidence Based Dentistry:
A study of 2000 cases showed that coronal coverage significantly improves the outcome of endodontic treatment., [2]. - This is why a crown was placed on the Re-RCT.
A prospective study of 771 adhesive bridges found that if RBB’s fail, they are most likely to fail within the first 4 years and very few fail thereafter with an estimated survival rate of 80.8% and 80.4% at 5 years and 10 years respectively [3]. - This shows that a RBB is a great minimally invasive way to restore a gap in a young patient.
The ideal occlusion for RBB’s should be organised so that the pontic has no contact in ICP and lateral excursions, [4]. - This is how I organised the patients occlusion.
Root filled teeth tend to make poor abutments, try to avoid where possible, [5].- This is why we did not use the Re-RCT UL5 as a bridge abutment.
Further Discussion:
UL5 was asymptomatic however, coronal coverage was indicated and I did not want to place a crown on a suboptimal root filling which is why I carried out the Re-RCT.
Challenging Re-RCT due to curvature of root.
Justified attempt since the end of the apex had not yet been reached.
Re-RCT achieved using flexible hand files.
Hand files helped maintain shape of curvature and avoid errors such as zipping or ledge.
Class 2 Division II incisor relationship protects this RBB due to the steep anterior guidance
Long term best option to replace edentulous space UL4 is an implant.
References:
Bsperio.org.uk (2016) The Good Practitioner’s Guide to Periodontology.
Imura, N., Pinheiro, E., Gomes, B., Zaia, A., Ferraz, C. and Souza-Filho, F. (2007). The Outcome of Endodontic Treatment: A Retrospective Study of 2000 Cases Performed by a Specialist. Journal of Endodontics 33(11), pp.1278-1282.
P.King, L.Foster, R.Yates,R.Newcombe and M.Garrett, (2015). “Survival characteristics of 771 resin retained bridges provided at a UK dental teaching hospital”. British Dental Journal, 218(7), pp.42-428.
Gulati, J, Tabiat-Pour, S, Watkins, S. and Banerjee, A, (2016). Resin-bonded bridges – the problem or the solution? part 1: assessment and design. Dental Update, 43(6), pp.506-521.
Zarow, M., Ramírez-Sebastià, A., Paolone, G., de Ribot Porta, J., Mora, J., Espona, J., Durán-Sindreu, F. and Roig, M. (2017). A new classification system for the restoration of root filled teeth. International Endodontic Journal, 51(3), pp.318-334.
Below is a poster of my case:

If you have any comments please comment below or message me.
I hope you enjoyed reading my case, thank you!





Phenomenal very proud!
A fantastic piece of work! Well done Payvand